![]() Free Shipping
Free Shipping ![]() Buy Now, Pay Later
Buy Now, Pay Later ![]() Eligible
Eligible
Blue Light Therapy for Fungal Infections: A Modern, Non-Invasive Treatment

Shedding New Light on Fungus: An Introduction to Blue Light Therapy
Fungal infections, from the common athlete’s foot to stubborn nail fungus (onychomycosis), affect millions worldwide. While topical creams and oral medications have been the standard treatment, they often come with limitations—side effects, long treatment times, and growing antifungal resistance. Enter Blue Light Therapy, an innovative, non-invasive treatment that is gaining traction in the dermatological world. This article illuminates how a specific wavelength of light is being harnessed to fight fungal pathogens effectively and safely.
How Does Blue Light Kill Fungus? The Science Explained
Blue light therapy does not rely on heat to destroy fungi. Instead, it utilizes a photodynamic effect. The key lies in certain molecules within the fungal cells called porphyrins.
- The Process: When blue light in a specific wavelength range (typically 405-470 nanometers) shines on the infection, it is absorbed by these natural porphyrins.
- The Reaction: This absorption of light energy excites the porphyrin molecules, causing them to produce reactive oxygen species (ROS), primarily singlet oxygen.
- The Result: These ROS molecules are highly toxic and cause oxidative damage to the fungal cell walls, membranes, and internal organelles, leading to the fungus’s death (apoptosis) without harming the surrounding human tissue.
Expert Insight: “Blue light therapy represents a paradigm shift in treating superficial fungal infections. It’s a physical modality, meaning there’s no risk of the fungus developing resistance as it might with repeated use of chemical antifungals. The targeted nature of the photodynamic effect makes it both effective and safe for patients,” explains Dr. Anya Sharma, a board-certified dermatologist.
Common Fungal Infections Treated with Blue Light
Blue light therapy has shown promising results in clinical studies for several common fungal conditions:
- Onychomycosis (Nail Fungus): A particularly stubborn infection to treat. Blue light devices, often designed as light pods or wands, can penetrate the nail plate to target the fungus underneath.
- Tinea Pedis (Athlete’s Foot): Effective at eliminating the fungus in the moist, warm environments between toes and on the soles of the feet.
- Tinea Corporis (Ringworm): Can be used to treat the characteristic ring-shaped rash on the body.
- Cutaneous Candidiasis: Useful for treating yeast infections on the skin.
Blue Light Therapy vs. Traditional Antifungal Treatments
How does this new technology stack up against the tried-and-true methods? The following table provides a clear comparison.
| Feature | Blue Light Therapy | Topical Antifungals (Creams) | Oral Antifungals (Pills) |
|---|---|---|---|
| Mechanism | Physical (Light Energy) | Chemical | Chemical |
| Invasiveness | Non-Invasive | Non-Invasive | Systemic (Internal) |
| Risk of Side Effects | Very Low (Local, temporary redness) | Low (Skin irritation) | Higher (Liver toxicity, drug interactions) |
| Risk of Resistance | Very Low | Possible | Yes (Growing concern) |
| Treatment Duration | Several sessions over weeks | Weeks to Months | Weeks to Months |
| Convenience | Home devices available | High | High |
| Cost | Higher upfront cost for devices | Low | Varies (with insurance) |
The Pros and Cons of Choosing Blue Light Therapy
Advantages of Blue Light Treatment
- Non-Invasive and Painless: The treatment is generally sensation-free, with no downtime required.
- No Drug Resistance: Since it’s a physical mechanism, fungi cannot become resistant to light therapy.
- Minimal Side Effects: The most common side effect is temporary, mild redness.
- Targeted Action: It selectively destroys fungal cells without damaging healthy skin.
- Suitable for Many Patients: A good option for those who cannot tolerate oral antifungal medications.
Limitations and Considerations
- Requires Multiple Sessions: Consistency is key. A full treatment course typically requires sessions several times a week for a number of weeks.
- Primarily for Superficial Infections: It is most effective for infections on or near the skin’s surface. Deep-seated systemic infections require different treatments.
- Cost of Devices: While clinical treatments are available, at-home devices can represent a significant initial investment.
- Not an Instant Cure: Results take time and patience, similar to most antifungal regimens.
What to Expect During a Blue Light Therapy Session
Whether in a clinic or at home, the process is straightforward:
- Cleaning: The affected area is thoroughly cleaned and dried.
- Exposure: The blue light device is positioned over the infection.
- Treatment: The light is activated for a predetermined time, usually a few minutes per area.
- Repetition: This process is repeated as per the prescribed schedule (e.g., twice daily for 4-6 weeks for a home device).
Patient Perspective: “After years of battling nail fungus with creams that didn’t work and being wary of oral medication, I tried a blue light device. It required discipline, but after three months, I finally saw clear, healthy nail growing in. It was a game-changer for me,” shares Mark T., a satisfied user.
The Future of Antifungal Treatment is Bright
Research into blue light therapy continues to expand. Scientists are exploring:
- Combination Therapies: Using blue light in conjunction with topical agents to enhance efficacy (antifungal photodynamic therapy).
- Optimizing Wavelengths: Fine-tuning specific light wavelengths to target different fungal species more effectively.
- Broader Applications: Investigating its use for other microbial skin conditions, like severe acne and bacterial infections.
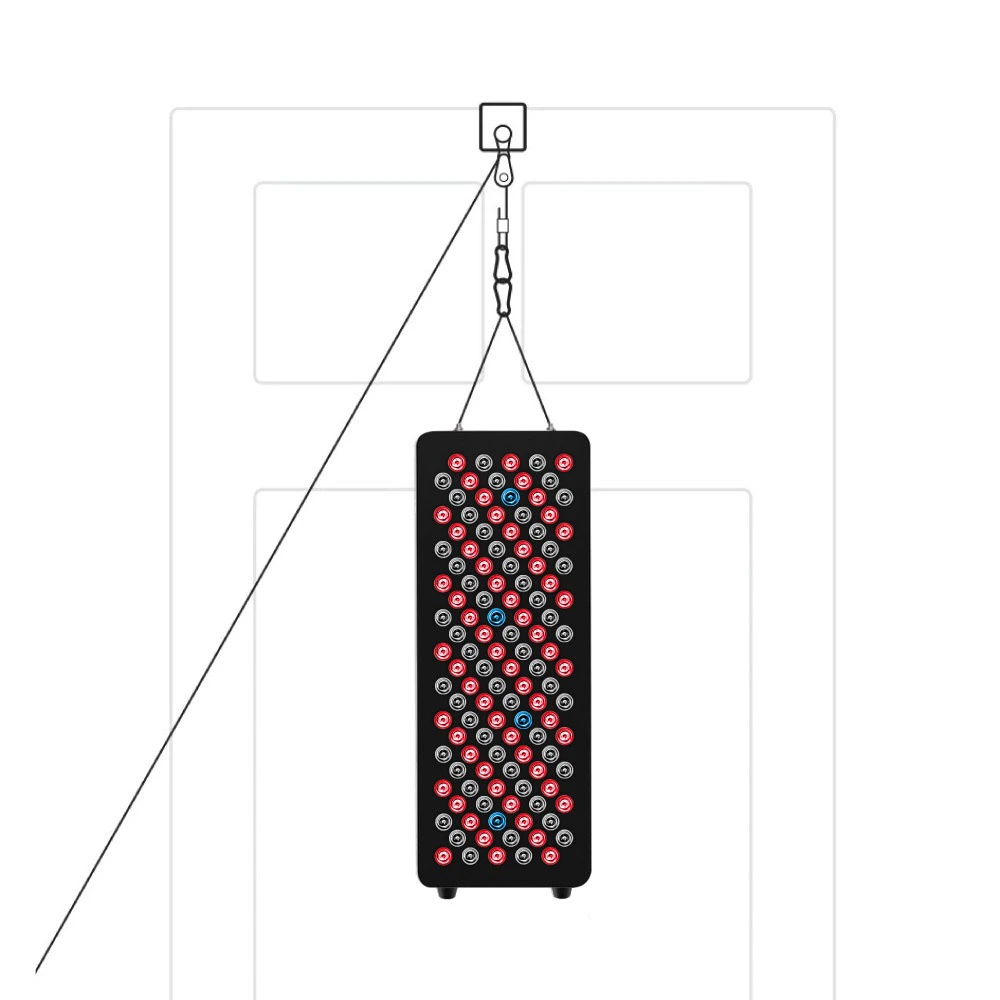
VELLGUS Elite V2
THE #1 RATED RED LIGHT DEVICE
VELLGUS pro V2
THE #1 RATED FULL BODY RED LIGHT DEVICE
Conclusion: Is Blue Light Therapy Right for You?
Blue light therapy presents a compelling, modern alternative for managing stubborn fungal skin and nail infections. Its non-invasive nature, excellent safety profile, and ability to bypass the issue of drug resistance make it a valuable tool in dermatology.
If you are frustrated with traditional treatments or are looking for a drug-free solution, consult your dermatologist or podiatrist. They can help you determine if blue light therapy is a suitable option for your specific condition and guide you on the best course of action, whether it’s an in-clinic procedure or a prescribed at-home device.