![]() Free Shipping
Free Shipping ![]() Buy Now, Pay Later
Buy Now, Pay Later ![]() Eligible
Eligible
Blue Light Therapy for Rosacea: A Soothing Guide to Calming Redness

Living with rosacea often means a constant battle against facial redness, visible blood vessels, and acne-like bumps. While traditional treatments like topical creams and oral antibiotics are common, many are now turning to a different kind of solution: blue light therapy. This non-invasive, gentle treatment is gaining traction for its ability to target the inflammatory components of rosacea effectively.
In this guide, we’ll illuminate how blue light therapy works, its specific benefits for rosacea sufferers, and what you can expect from a treatment course.
What is Blue Light Therapy and How Does It Work for Rosacea?
Blue light therapy falls under the category of photodynamic therapy (PDT) or light-emitting diode (LED) therapy. It utilizes specific wavelengths of blue light, typically in the 405-420 nanometer range, to target and destroy bacteria and calm inflammation on the skin.
For rosacea, the mechanism is two-fold:
- Antibacterial Action: While rosacea isn’t caused by bacteria in the same way as common acne, the Demodex folliculorum mite and the bacteria associated with it are often found in higher numbers on rosacea-prone skin. Blue light has an antibacterial effect, helping to reduce the population of these mites and their associated inflammation.
- Anti-Inflammatory Effects: The blue light penetrates the skin and is absorbed by molecules within skin cells. This process can help calm the underlying inflammation that leads to the persistent redness and papules (bumps) characteristic of rosacea.
Expert Insight: “Blue light therapy offers a unique, non-antibiotic approach to managing the inflammatory lesions of rosacea. It targets the microscopic Demodex mites and associated bacteria, which are known contributors to the papulopustular flares of the condition, providing relief without the risk of antibiotic resistance.” – Hypothetical Dermatology Expert
The Key Benefits of Choosing Blue Light for Rosacea
Why consider blue light therapy? The advantages are particularly appealing for those with sensitive skin who may not tolerate stronger medications or lasers.
- Non-Invasive and Gentle: There are no needles, incisions, or downtime. The procedure is often described as a warm, gentle light on the skin.
- Targets Inflammation: Directly addresses the red, angry bumps (papulopustular rosacea) by calming the skin at a cellular level.
- Reduces Reliance on Medication: It can be an excellent option for patients looking to reduce their use of topical or oral antibiotics.
- Minimal Side Effects: The most common side effect is temporary, mild dryness or redness immediately after treatment.
- Safe for Most Skin Types: It is generally safe for a wide range of skin tones.
What to Expect During a Blue Light Therapy Session
Understanding the process can help alleviate any anxiety. A typical in-office treatment follows these steps:
- Consultation: A dermatologist will assess your skin to confirm you are a good candidate.
- Cleansing: Your face will be thoroughly cleansed to remove any makeup, oil, or sunscreen.
- Protection: You will be given special goggles to protect your eyes from the bright light.
- Treatment: You will sit or lie down while a blue light device is positioned over your face. The treatment usually lasts between 15-30 minutes.
- Post-Treatment Care: The practitioner will apply a gentle moisturizer and sunscreen. You can resume most normal activities immediately.
A course of treatment is usually necessary for optimal results, often involving 2-3 sessions per week for several weeks.
Blue Light vs. Other Rosacea Treatments: A Comparative Look
Blue light therapy is just one tool in the arsenal against rosacea. Here’s how it compares to other common treatments.
| Treatment Type | How It Works | Best For | Pros | Cons |
|---|---|---|---|---|
| Blue Light Therapy | Uses LED light to kill bacteria & reduce inflammation. | Papulopustular rosacea (redness with bumps). | Non-invasive, no downtime, minimal side effects. | Requires multiple sessions, less effective for visible blood vessels. |
| Topical Medications (e.g., Metronidazole, Ivermectin) | Applied directly to skin to reduce inflammation & Demodex. | Mild to moderate redness and bumps. | Easy to use at home, prescribed by a doctor. | Can cause skin irritation, dryness, or burning. |
| Oral Antibiotics (e.g., Doxycycline) | Systemic reduction of inflammation. | Moderate to severe inflammatory rosacea. | Powerful for significant flares. | Risk of side effects (upset stomach, sun sensitivity), antibiotic resistance. |
| IPL/Laser Therapy | Uses intense light/beam to target blood vessels & redness. | Erythematotelangiectatic rosacea (redness & visible veins). | Highly effective for permanent redness and broken capillaries. | More expensive, can require downtime, risk of bruising. |
Potential Side Effects and Who Should Avoid It
Blue light therapy is exceptionally safe. However, some individuals may experience:
- Temporary redness, dryness, or slight swelling.
- A sensation of tightness in the skin for a few hours.
- In rare cases, temporary pigment changes.
It may not be suitable for people with photosensitive conditions (like lupus), those taking photosensitizing medications, or individuals with a history of skin cancer. A consultation with a dermatologist is essential.
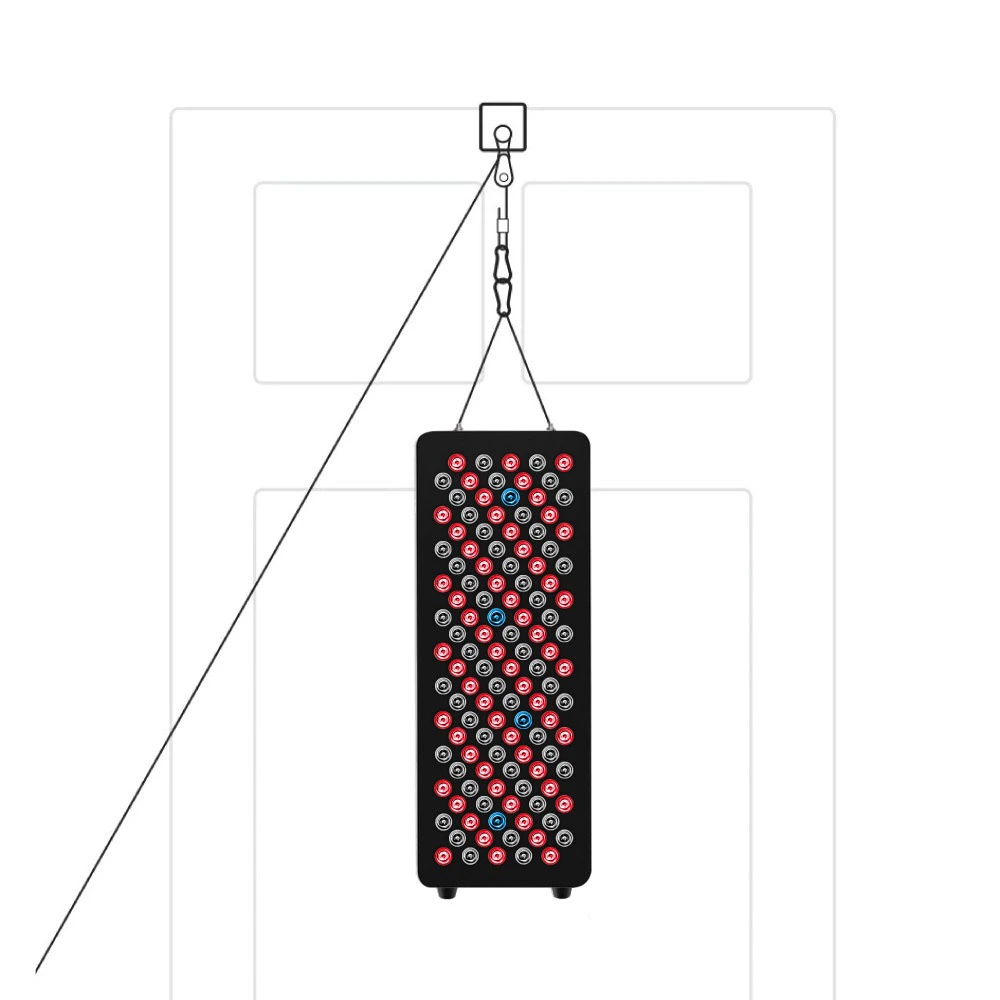
VELLGUS Elite V2
THE #1 RATED RED LIGHT DEVICE
VELLGUS pro V2
THE #1 RATED FULL BODY RED LIGHT DEVICE
Is Blue Light Therapy Right for Your Rosacea?
Blue light therapy presents a compelling, low-risk option for managing the inflammatory symptoms of rosacea. It works best as part of a comprehensive skincare and consistent use.
If you are frustrated with traditional creams and pills or are looking for a gentle yet effective treatment, discussing blue light therapy with your skin specialist could be the next step toward calmer, clearer skin.