![]() Free Shipping
Free Shipping ![]() Buy Now, Pay Later
Buy Now, Pay Later ![]() Eligible
Eligible
Blue Light Therapy for Seborrheic Dermatitis: A Comprehensive Guide

Seborrheic dermatitis is a common, frustrating skin condition that causes red, itchy, and flaky patches, often on the scalp (as dandruff), face, and chest. While traditional treatments like medicated shampoos and topical steroids can be effective, they don’t work for everyone and can come with side effects. Enter blue light therapy—a promising, non-invasive treatment gaining traction in dermatology. This article explores how blue light therapy works for seborrheic dermatitis, its benefits, and how it compares to other treatments.
What is Seborrheic Dermatitis?
Before diving into the treatment, it’s crucial to understand the enemy. Seborrheic dermatitis is a chronic inflammatory condition. Its exact cause is multifactorial, but key players include:
- An Overgrowth of Yeast: The yeast Malassezia is a natural resident on our skin, but in some individuals, it overgrows, triggering an inflammatory response.
- Excess Sebum Production: Oily skin (seborrhea) provides the perfect food source for Malassezia.
- Individual Susceptibility: Factors like stress, hormones, and a compromised immune system can make someone more prone to flare-ups.
How Does Blue Light Therapy Work?
Blue light therapy, also known as phototherapy, utilizes a specific wavelength of light in the blue spectrum (typically around 415 nanometers) to target the root causes of seborrheic dermatitis.
The Science Behind the Light
Blue light works through two primary mechanisms:
- Antimicrobial Action: The blue wavelength is naturally absorbed by molecules called porphyrins, which are produced by the Malassezia yeast. When light is absorbed, it creates a toxic reaction within the yeast cells, effectively killing them and reducing their population on the skin.
- Anti-Inflammatory Effects: By reducing the yeast overgrowth, blue light indirectly calms the inflammation they cause. There is also evidence that light in the blue spectrum can directly modulate immune responses in the skin, further reducing redness and swelling.
Expert Insight: “Blue light therapy offers a unique advantage by targeting the Malassezia yeast without the use of pharmaceuticals. This makes it an excellent option for patients looking for a non-invasive treatment or those who have not responded well to topical antifungals,” explains a typical statement from a consulting dermatologist.
Benefits of Using Blue Light for Seborrheic Dermatitis
Why choose blue light over a bottle of shampoo? The benefits are compelling:
- Non-Invasive and Drug-Free: It’s a physical treatment, not a chemical one. This eliminates the risk of systemic side effects or skin thinning associated with prolonged steroid use.
- Targets the Root Cause: Unlike some treatments that just slough off scales, blue light directly addresses the microbial imbalance.
- Minimal Side Effects: The most common side effect is temporary, mild dryness or redness, which typically resolves quickly.
- Suitable for Sensitive Skin: It can be used on delicate areas like the face, hairline, and chest where stronger topical treatments might be too irritating.
- Complements Other Treatments: It can be used alongside your existing skincare routine to enhance overall results.
Blue Light Therapy vs. Other Treatments
How does blue light stack up against the classics? The table below provides a clear comparison.
| Treatment Method | How It Works | Pros | Cons |
|---|---|---|---|
| Blue Light Therapy | Kills Malassezia yeast with specific light wavelengths. | Non-invasive, minimal side effects, drug-free, targets root cause. | Requires multiple sessions, can be costly, less accessible. |
| Topical Antifungals (e.g., Ketoconazole) | Directly inhibits yeast growth. | Widely available, effective for many, inexpensive. | Can cause skin irritation, yeast can develop resistance over time. |
| Topical Corticosteroids (e.g., Hydrocortisone) | Suppresses inflammation quickly. | Fast-acting for redness and itching. | Risk of skin thinning, rebound flares, not for long-term use. |
| Medicated Shampoos (e.g., Zinc Pyrithione, Selenium Sulfide) | Anti-fungal and anti-scaling action. | Over-the-counter, easy to use for scalp SD. | Can be drying, may lose effectiveness, often only manages symptoms. |
| Coal Tar & Salicylic Acid | Slows skin cell growth and loosens scales. | Effective exfoliation, reduces scaling. | Strong odor, can stain hair/skin, potentially irritating. |
What to Expect During Treatment
Blue light therapy can be administered in a dermatologist’s office or at home with FDA-cleared devices.
In-Office Treatments
A clinical session involves sitting in front of a panel of blue lights for a short, prescribed period (usually 15-30 minutes). A typical course might require 2-3 sessions per week for several weeks to see significant improvement.
At-Home Devices
The market now offers handheld blue light devices, masks, and even combs for the scalp. These are convenient but typically less powerful than clinical units. Consistency is key with at-home treatment.
User Experience Quote: “After years of cycling through different shampoos and creams, I was skeptical. But using a blue light comb for my scalp dermatitis for just a few weeks made a visible difference. The itching reduced first, and then the flaking started to calm down,” shares a typical user review.
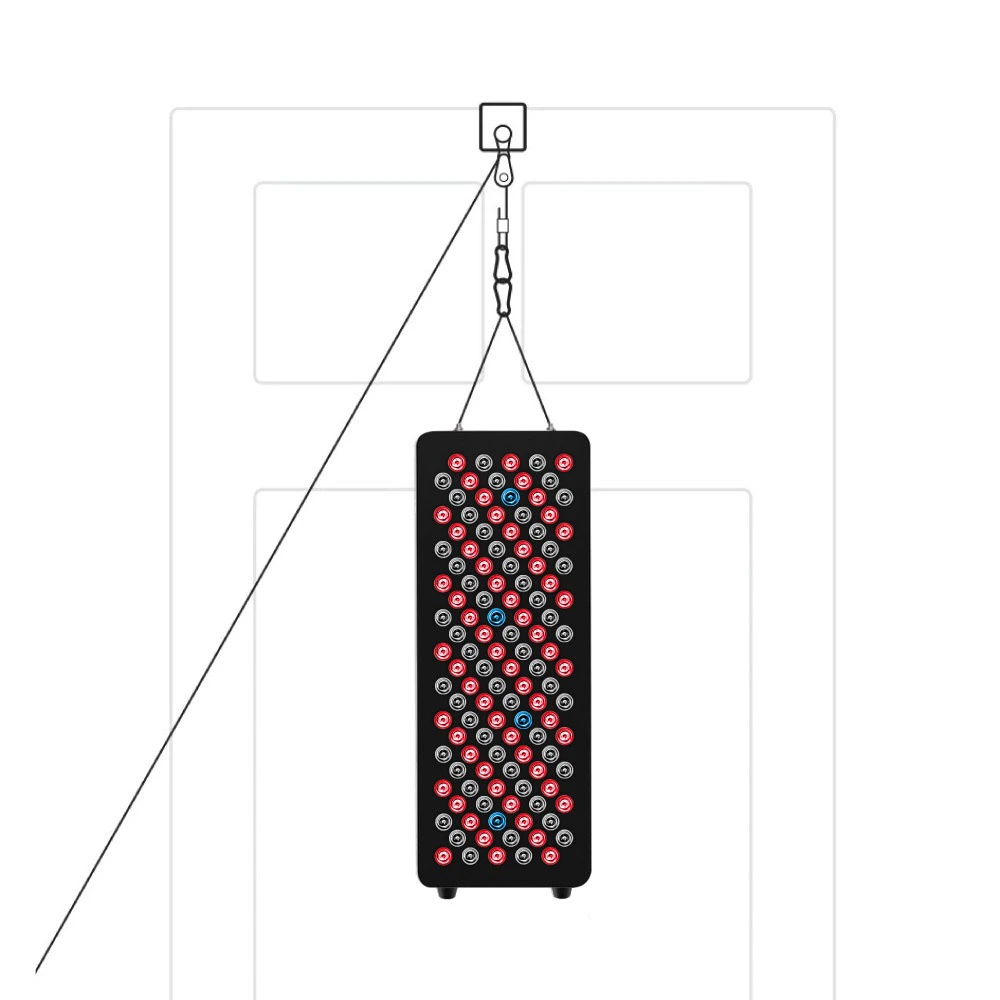
VELLGUS Elite V2
THE #1 RATED RED LIGHT DEVICE
VELLGUS pro V2
THE #1 RATED FULL BODY RED LIGHT DEVICE
Potential Side Effects and Considerations
Blue light therapy is considered very safe. However, it’s not for everyone.
- Side Effects: Temporary dryness, redness, or slight tenderness are possible but rare.
- Contraindications: Individuals who are photosensitive or taking photosensitizing medications should avoid this therapy.
- Consult a Professional: It is always recommended to speak with a dermatologist before starting any new treatment to ensure it’s the right choice for your specific condition.
Conclusion: Is Blue Light Therapy Right for You?
Blue light therapy represents a significant advancement in managing seborrheic dermatitis. By offering a non-invasive, drug-free, and targeted approach, it fills an important gap in treatment options, especially for those with resistant cases or sensitive skin.
While it may require an initial investment of time and money, the potential for long-term control without the side effects of traditional medications is a powerful benefit. If you are struggling to keep your seborrheic dermatitis under control, discussing blue light therapy with your dermatologist could be the illuminating solution you’ve been searching for.