![]() Free Shipping
Free Shipping ![]() Buy Now, Pay Later
Buy Now, Pay Later ![]() Eligible
Eligible
Blue Light Therapy for Skin Cancer: A Comprehensive Guide to the Pros and Cons

When you hear the words “skin cancer treatment,” your mind might immediately go to surgery or radiation. But what if a non-invasive, light-based treatment could effectively target and destroy certain cancerous cells? Enter Photodynamic Therapy (PDT), often referred to by its most common type: Blue Light Therapy.
This innovative treatment is gaining traction, but is it the right choice for you? In this detailed guide, we’ll illuminate the pros and cons of blue light therapy, helping you make an informed decision alongside your dermatologist.
What is Blue Light Therapy (Photodynamic Therapy)?
Blue Light Therapy is a two-step medical treatment used to treat certain types of pre-cancers and early-stage skin cancers, as well as severe sun damage. It’s a form of Photodynamic Therapy (PDT) that uses a specific wavelength of blue light to activate a photosensitizing drug applied to the skin.
The process works like this:
- Application: A topical photosensitizing agent, most often Aminolevulinic Acid (ALA), is applied to the target area.
- Incubation: The area is covered and left for a period (typically 1-3 hours) to allow the medication to be absorbed by the abnormal skin cells.
- Activation: The area is then exposed to a specific blue light wavelength. This light activates the drug, causing a chemical reaction that destroys the targeted cells.
Quote from an Expert:
“Think of Photodynamic Therapy as a targeted missile system. We apply a substance that is preferentially absorbed by rapidly dividing, abnormal cells. The blue light is the ‘launch code’ that triggers a reaction, creating oxygen free radicals that precisely destroy those cells while sparing the surrounding healthy tissue.”
— Dr. Sarah Jenkins, MD, Board-Certified Dermatologist
The Pros: Benefits of Blue Light Therapy for Skin Cancer
Blue Light Therapy offers several significant advantages, especially for treating widespread sun damage and superficial cancers.
✅ Non-Invasive and Excellent Cosmetic Results
Unlike surgical excision, PDT does not involve cutting or stitching. This makes it an excellent option for areas where cosmetic outcome is a priority, such as the face, ears, and neck. It typically results in minimal scarring.
✅ Effectively Treats Large or Multiple Areas
Because the photosensitizer is a cream or liquid, it can be applied to large areas of the body. This is a major advantage for patients with Field Cancerization—widespread pre-cancerous changes (Actinic Keratoses) across the scalp, face, or arms.
✅ High Efficacy for Precancerous Lesions
PDT is FDA-approved and highly effective at clearing Actinic Keratoses (AKs), which are considered the earliest stage of squamous cell carcinoma. Studies show clearance rates often exceeding 90% for these pre-cancers.
✅ Can Reduce Future Skin Cancer Risk
By treating an entire “field” of sun-damaged skin, blue light therapy doesn’t just address visible lesions; it can also treat microscopic pre-cancers that haven’t yet surfaced, potentially reducing the risk of developing new skin cancers in that area in the future.
✅ Minimal Downtime (Compared to Surgery)
The procedure is typically done in a dermatologist’s office and does not require general anesthesia. While there is a recovery period (which we’ll cover in the cons), patients can usually return to normal, non-strenuous activities the next day.
The Cons: Drawbacks and Side Effects of Blue Light Therapy
While powerful, blue light therapy is not a one-size-fits-all solution and comes with its own set of challenges.
❌ Not Suitable for All Skin Cancers
This is the most critical limitation. Blue light therapy is primarily for:
- Actinic Keratoses (AKs)
- Superficial Basal Cell Carcinoma
It is not recommended for thicker Basal Cell Carcinomas, Squamous Cell Carcinomas, or Melanoma, where surgical excision remains the gold standard for complete removal and accurate staging.
❌ Significant Pain and Discomfort During Treatment
The light activation phase can be intensely painful for many patients, described as a severe burning, stinging, or prickling sensation. While the pain usually subsides shortly after the light is turned off, it can be a major deterrent.
❌ Stringent Post-Treatment Light Avoidance
After the procedure, the photosensitizing drug remains active in your skin for 24-48 hours. You must strictly avoid direct sunlight and even bright indoor light to prevent a severe sunburn-like reaction. This can be highly disruptive to your daily life.
❌ The “Ugly Duckling” Phase and Recovery
Treated areas become red, swollen, and form crusts and scales before they heal. This recovery period, often called the “PDT reaction,” can last 1-2 weeks and can be cosmetically challenging to manage.
❌ Often Requires Multiple Sessions
While a single treatment can be effective, many dermatologists recommend two treatments spaced a few weeks apart for the best clearance rates of AKs, meaning more time, cost, and discomfort.
Blue Light Therapy vs. Other Common Treatments: A Quick Comparison
The table below provides a high-level comparison to help you understand where PDT fits among other standard treatments.
| Feature | Blue Light Therapy (PDT) | Surgical Excision | Cryotherapy (Freezing) | Topical Creams (e.g., 5-FU, Imiquimod) |
|---|---|---|---|---|
| Best For | Superficial BCC, widespread AKs | Invasive BCC, SCC, Melanoma | Isolated, few AKs | Small areas of AKs |
| Invasiveness | Non-invasive | Invasive (cutting) | Minimally invasive | Non-invasive |
| Pain Level | High during treatment | Moderate (with local anesthesia) | Moderate (stinging) | Moderate (irritation) |
| Scarring | Minimal | Yes (linear scar) | Possible (white spot) | Minimal |
| Downtime | 1-2 weeks (recovery phase) | 1-2 weeks | 1-2 weeks | Several weeks |
| Cost | Moderate to High | High | Low | Low to Moderate |
Quote from an Expert:
“The decision between PDT, surgery, or a topical treatment is a nuanced one. We consider the type and depth of the cancer, its location, the patient’s overall skin condition, and their tolerance for recovery. For a patient with dozens of pre-cancers on their face, PDT is a game-changer. For a single, thick basal cell carcinoma on the back, surgery is unequivocally the better choice for a cure.”
— Dr. Michael Chen, MD, Mohs Surgeon
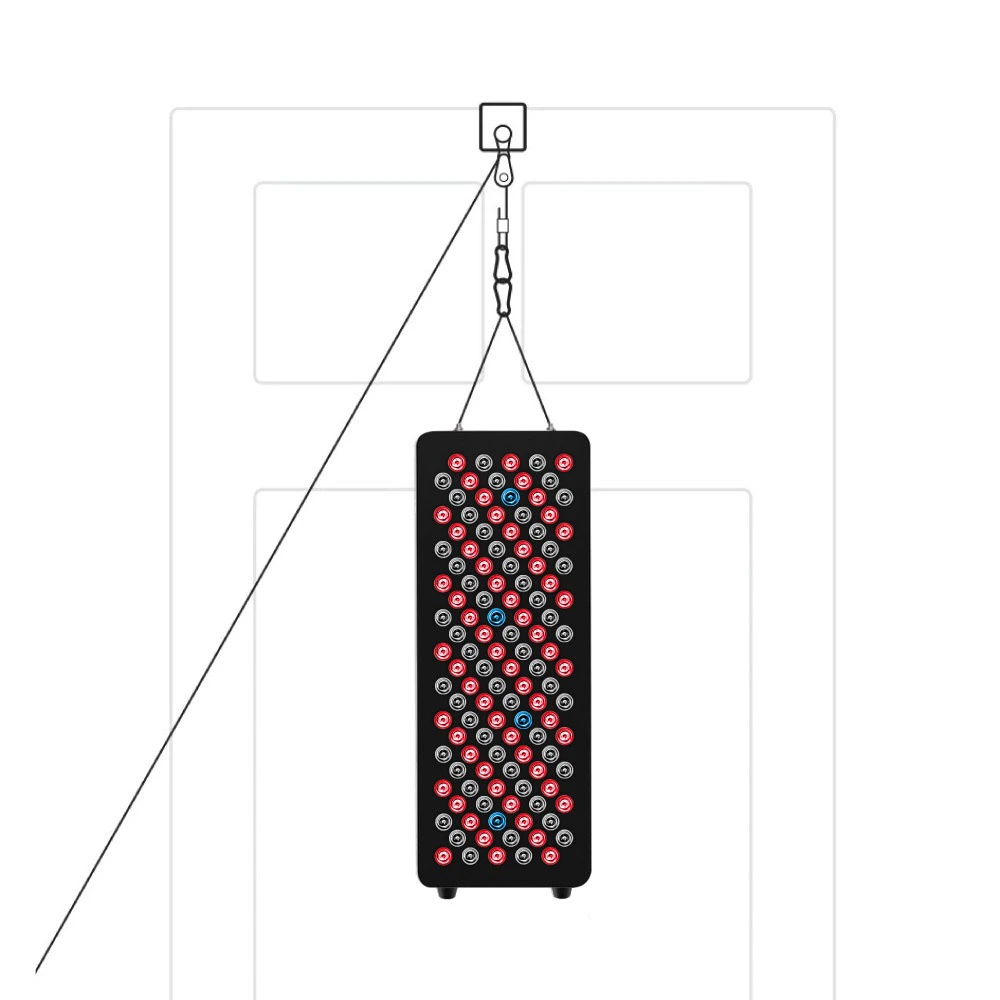
VELLGUS Elite V2
THE #1 RATED RED LIGHT DEVICE
VELLGUS pro V2
THE #1 RATED FULL BODY RED LIGHT DEVICE
Is Blue Light Therapy Right for You? The Bottom Line
Blue Light Therapy (PDT) is a powerful, FDA-approved tool in the fight against skin cancer, but it has a very specific role. Its greatest strength lies in treating widespread pre-cancerous actinic keratoses and superficial basal cell carcinomas with excellent cosmetic outcomes.
However, its limitations are significant. It is not a substitute for surgery for more invasive cancers, the treatment itself can be painful, and the post-procedure light sensitivity requires serious commitment.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare professional for diagnosis and before starting any new treatment.