![]() Free Shipping
Free Shipping ![]() Buy Now, Pay Later
Buy Now, Pay Later ![]() Eligible
Eligible
Red Light Therapy for Diabetic Ulcers: Promoting Healing and Reducing Complications

Diabetes is a chronic condition affecting millions worldwide, with complications that can severely impact quality of life. One of the most challenging complications is diabetic ulcers—chronic wounds that often resist healing and can lead to severe infections, amputations, and even death. Traditional treatments, including wound debridement, antibiotics, and advanced dressings, have limitations, prompting researchers to explore alternative therapies.
Among these emerging treatments, red light therapy (RLT), also known as low-level laser therapy (LLLT) or photobiomodulation, has shown remarkable promise in accelerating wound healing and reducing complications in diabetic ulcers. This article explores how red light therapy works, its benefits for diabetic ulcers, scientific evidence supporting its use, and practical considerations for patients and healthcare providers.
Understanding Diabetic Ulcers
What Are Diabetic Ulcers?
Diabetic ulcers are open sores or wounds that commonly occur on the feet of individuals with diabetes. They result from a combination of factors, including:
- Poor circulation (peripheral arterial disease)
- Nerve damage (neuropathy), reducing sensation and delaying injury detection
- High blood sugar levels, impairing immune function and wound repair
Without proper treatment, these ulcers can become infected, leading to osteomyelitis (bone infection), gangrene, and the need for amputation.
Current Treatment Challenges
Standard treatments include:
- Wound debridement (removing dead tissue)
- Antibiotics for infections
- Offloading pressure (special footwear or casts)
- Advanced wound dressings (hydrogels, collagen-based products)
Despite these methods, many ulcers remain chronic and non-healing, necessitating alternative approaches like red light therapy.
What Is Red Light Therapy?
Red light therapy (RLT) involves exposing the skin to low-wavelength red or near-infrared light (600–1000 nm). Unlike UV light, which can damage skin, RLT is non-invasive, painless, and free of harmful side effects.
How Does It Work?
RLT works at a cellular level, stimulating mitochondria (the cell’s energy powerhouse) to produce more adenosine triphosphate (ATP). Increased ATP enhances cell repair, regeneration, and overall metabolic activity.
Key mechanisms in wound healing include:
- Enhanced Collagen Production – Promotes tissue repair.
- Reduced Inflammation – Lowers pro-inflammatory cytokines.
- Improved Blood Flow – Stimulates angiogenesis (new blood vessel formation).
- Antimicrobial Effects – Helps combat infections.
- Stem Cell Activation – Encourages tissue regeneration.
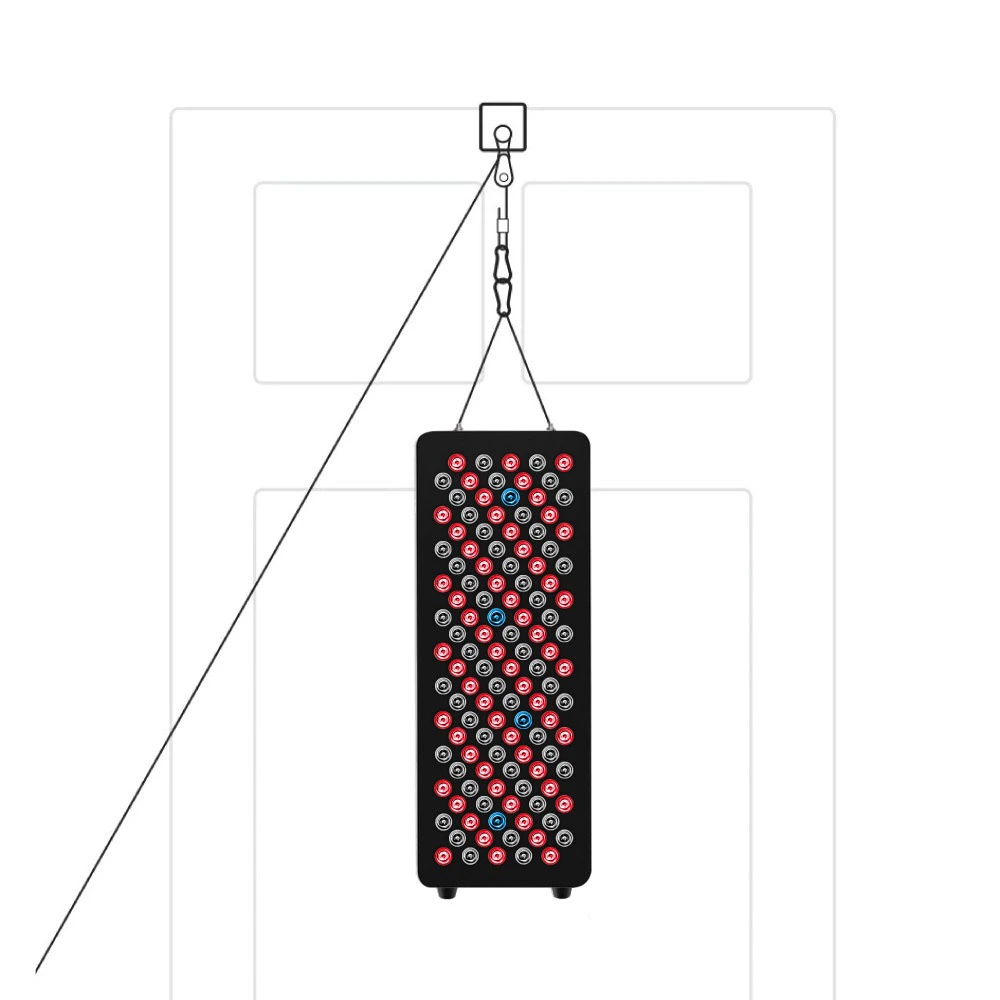
VELLGUS Elite V2
THE #1 RATED RED LIGHT DEVICE
VELLGUS pro V2
THE #1 RATED FULL BODY RED LIGHT DEVICE
Scientific Evidence: Red Light Therapy for Diabetic Ulcers
Clinical Studies Supporting RLT
Multiple studies have demonstrated the effectiveness of RLT in diabetic wound healing:
- 2014 Study (Diabetes Research and Clinical Practice)
- Patients with diabetic foot ulcers received near-infrared light therapy.
- Results: 40% faster healing compared to standard care alone.
- 2018 Meta-Analysis (Journal of Diabetes Science and Technology)
- Reviewed 12 clinical trials on photobiomodulation for diabetic ulcers.
- Conclusion: Significant improvement in wound closure rates with RLT.
- 2020 Randomized Controlled Trial (Lasers in Medical Science)
- Compared RLT + standard care vs. standard care alone.
- Findings: RLT group had 50% faster healing and fewer infections.
Why Is RLT Particularly Effective for Diabetic Ulcers?
Diabetes impairs:
- Fibroblast activity (cells that produce collagen)
- Circulation (reducing oxygen and nutrient delivery)
- Immune response (increasing infection risk)
RLT counters these effects by:
✔ Boosting cellular energy (ATP) for faster repair.
✔ Increasing nitric oxide, improving blood flow.
✔ Reducing oxidative stress, a major factor in diabetic complications.
Practical Applications: How to Use RLT for Diabetic Ulcers
Professional vs. At-Home Treatments
- Clinical Settings (Doctors, Wound Care Centers)
- Uses medical-grade laser or LED devices.
- Typically administered 2-3 times per week.
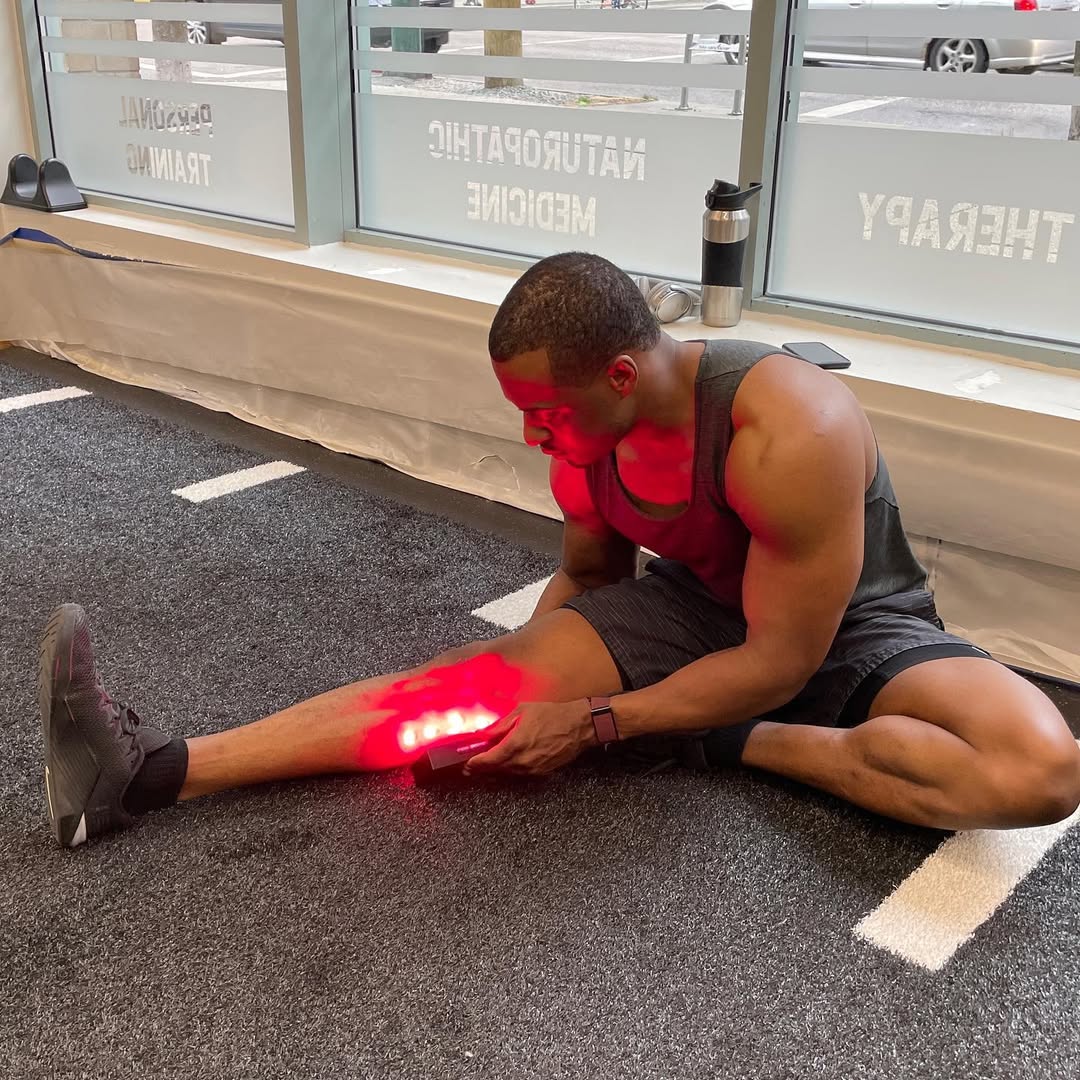
- At-Home Devices
- FDA-cleared red light therapy panels or handheld devices.
- Must follow proper wavelength (630–850 nm) and dosage guidelines.
Treatment Protocol
- Wavelength: 630–850 nm (red to near-infrared).
- Duration: 5–20 minutes per session.
- Frequency: 3–5 times per week.
- Safety: Avoid direct exposure to eyes; consult a doctor before use.
Combining RLT with Other Therapies
For best results, RLT can be combined with:
- Offloading devices (to reduce pressure).
- Advanced dressings (hydrocolloids, silver-based).
- Blood sugar control (critical for healing).
Patient Success Stories
Case Study 1: John’s Recovery from a Non-Healing Ulcer
John, a 62-year-old diabetic, had a foot ulcer for 8 months without improvement. After 6 weeks of RLT treatments, his wound reduced in size by 70%, and he avoided amputation.
Case Study 2: Maria’s Faster Healing Post-Surgery
Maria developed an ulcer after minor foot surgery. With RLT + standard care, her wound healed in 4 weeks instead of the projected 12.
Potential Risks and Limitations
While RLT is generally safe, considerations include:
- Overuse (can cause temporary redness).
- Improper wavelength (may reduce effectiveness).
- Not a standalone cure (must be combined with diabetes management).
Future of RLT in Diabetic Wound Care
Researchers are exploring:
- Wearable RLT devices for continuous treatment.
- Combination therapies (RLT + stem cells, growth factors).
- Personalized light dosages based on wound severity.
Conclusion: A Promising Adjunct Therapy
Red light therapy offers a safe, non-invasive, and scientifically backed method to enhance diabetic ulcer healing. By stimulating cellular repair, reducing inflammation, and improving circulation, RLT can reduce complications, prevent amputations, and improve quality of life for diabetic patients.
If you or a loved one suffers from a diabetic ulcer, consult a healthcare provider about integrating red light therapy into your treatment plan. With continued research, RLT may soon become a standard therapy in diabetic wound care.