![]() Free Shipping
Free Shipping ![]() Buy Now, Pay Later
Buy Now, Pay Later ![]() Eligible
Eligible
Red Light Therapy for Diabetic Ulcers: Promoting Healing and Reducing Complications
Diabetes is a chronic condition affecting millions worldwide, and one of its most challenging complications is the development of diabetic ulcers. These slow-healing wounds, often found on the feet, can lead to severe infections, amputations, and even death if not properly managed. Traditional treatments like wound debridement, antibiotics, and specialized dressings help, but they don’t always guarantee complete healing.
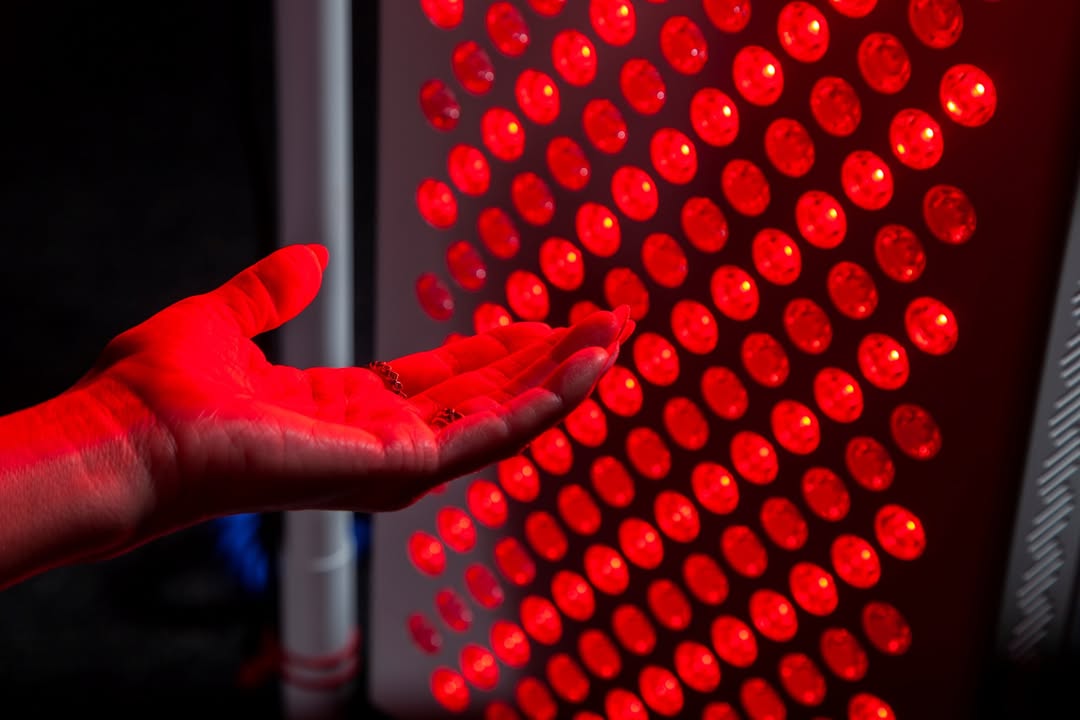
Enter red light therapy (RLT), a non-invasive, painless treatment that harnesses the power of low-wavelength red and near-infrared light to stimulate cellular repair. Could this be the breakthrough diabetic patients have been waiting for? Let’s explore how RLT works, its benefits for diabetic ulcers, and what the latest research says.
Understanding Diabetic Ulcers: Why Are They So Hard to Heal?
Before diving into red light therapy, it’s crucial to understand why diabetic ulcers are such a persistent problem.
Key Factors Contributing to Poor Wound Healing in Diabetes:
- Poor Circulation (Peripheral Artery Disease) – High blood sugar damages blood vessels, reducing blood flow to extremities.
- Neuropathy (Nerve Damage) – Loss of sensation means patients may not notice injuries until they become severe.
- Chronic Inflammation – Diabetes disrupts the body’s natural healing processes, leading to prolonged inflammation.
- Higher Infection Risk – Elevated glucose levels create an ideal environment for bacterial growth.
Conventional treatments focus on wound care, offloading pressure, and infection control, but they don’t always address the underlying cellular dysfunction. This is where red light therapy comes in.
What Is Red Light Therapy (RLT)?
Red light therapy, also known as low-level laser therapy (LLLT) or photobiomodulation (PBM), uses specific wavelengths of red (630-700 nm) and near-infrared (700-1100 nm) light to penetrate the skin and stimulate cellular energy production.
How Does It Work?
- Boosts Mitochondrial Function – Light energy is absorbed by mitochondria (the cell’s powerhouses), increasing ATP (adenosine triphosphate) production, which fuels cell repair.
- Reduces Inflammation – Modulates cytokines, decreasing chronic inflammation that hinders healing.
- Enhances Collagen Production – Stimulates fibroblasts, the cells responsible for creating new tissue.
- Improves Blood Flow – Promotes angiogenesis (formation of new blood vessels), crucial for wound healing.
Unlike UV light, RLT doesn’t damage the skin—it energizes and repairs it.
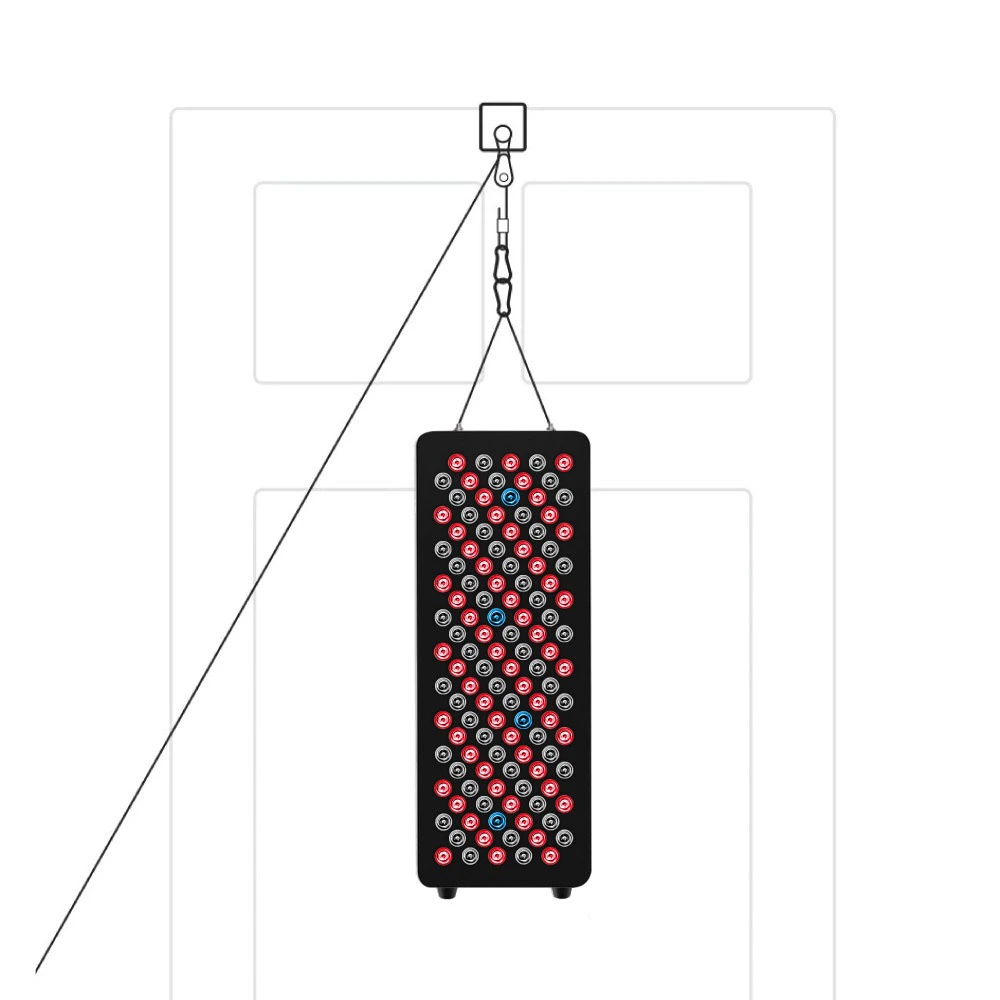
VELLGUS Elite V2
THE #1 RATED RED LIGHT DEVICE
VELLGUS pro V2
THE #1 RATED FULL BODY RED LIGHT DEVICE
Can Red Light Therapy Really Help Diabetic Ulcers?
What the Research Says
Several studies suggest RLT can significantly improve diabetic wound healing:
- 2014 Study (Diabetes & Metabolism Journal) – Found that near-infrared light therapy accelerated wound closure in diabetic rats by enhancing collagen synthesis and reducing oxidative stress.
- 2017 Clinical Trial (Journal of Diabetes Research) – Patients with diabetic foot ulcers receiving RLT showed faster healing rates and lower infection risks compared to standard care alone.
- 2020 Meta-Analysis (Lasers in Medical Science) – Concluded that photobiomodulation significantly improved wound healing in diabetic patients, with minimal side effects.
Real-World Benefits for Diabetics
- Faster Wound Closure – Some studies report up to 30-50% faster healing.
- Reduced Risk of Amputation – By preventing infections and promoting tissue regeneration.
- Pain Relief – Helps alleviate neuropathic pain associated with ulcers.
- Non-Invasive & Safe – No burns, scars, or downtime.
How to Use Red Light Therapy for Diabetic Ulcers
RLT can be administered in clinics or at home with FDA-cleared devices. Here’s how it’s typically applied:
- Professional Treatment – Wound care specialists may use medical-grade lasers or LED panels for targeted therapy.
- At-Home Devices – Portable red light therapy lamps or wraps allow daily treatment (always consult a doctor first).
- Treatment Protocol – Sessions usually last 5-20 minutes, applied 3-5 times per week until healing improves.
Precautions
- Always consult a healthcare provider before starting RLT.
- Avoid using on actively infected wounds without antibiotic treatment.
- Monitor blood sugar levels, as improved healing may affect diabetes management.
The Future of RLT in Diabetic Wound Care
With increasing research supporting its benefits, red light therapy could become a standard adjunct treatment for diabetic ulcers. Some exciting developments include:
- Combination Therapies – RLT paired with stem cell treatments or growth factor therapy.
- Wearable Light Devices – Smart bandages with embedded LEDs for continuous healing.
- Personalized Wavelengths – Optimizing light spectra for individual patient needs.
Final Thoughts: Is Red Light Therapy Worth Trying?
For diabetics struggling with chronic ulcers, red light therapy offers a safe, drug-free, and scientifically backed option to enhance healing. While it’s not a standalone cure, its ability to reduce inflammation, boost cell repair, and improve circulation makes it a promising tool in wound management.
If you or a loved one is battling diabetic ulcers, ask your doctor about incorporating RLT into your treatment plan. The future of wound care is bright—literally!
Have you tried red light therapy for wound healing? Share your experiences in the comments!
References & Further Reading
- Hamblin, M. R. (2017). Mechanisms and applications of the anti-inflammatory effects of photobiomodulation. AIMS Biophysics.
- Minatel, D. G. (2009). Phototherapy improves healing of chronic venous ulcers. Photomedicine and Laser Surgery.
- Zarei, M. (2020). Therapeutic outcomes of photobiomodulation in diabetic wound healing: A systematic review. Lasers in Medical Science.