![]() Free Shipping
Free Shipping ![]() Buy Now, Pay Later
Buy Now, Pay Later ![]() Eligible
Eligible
Red Light Therapy for Treating Pancreatitis: Facts and Studies

Pancreatitis—a painful and potentially life-threatening inflammation of the pancreas—affects millions of people worldwide. Traditional treatments include pain management, enzyme supplements, dietary changes, and, in severe cases, surgery. However, emerging research suggests that red light therapy (RLT), also known as photobiomodulation (PBM), may offer a promising non-invasive treatment option.
But can red light therapy really help with pancreatitis? What does the science say? In this comprehensive guide, we’ll explore:
- The science behind red light therapy
- How it may benefit pancreatitis patients
- Key studies supporting its use
- Practical ways to incorporate RLT into treatment
- Safety considerations
Whether you’re a patient, caregiver, or health enthusiast, this article will provide valuable insights into this cutting-edge therapy.
Understanding Pancreatitis: Causes and Challenges
Before diving into red light therapy, it’s essential to understand pancreatitis itself.
What Is Pancreatitis?
Pancreatitis is the inflammation of the pancreas, an organ responsible for:
- Producing digestive enzymes
- Regulating blood sugar via insulin and glucagon
When inflamed, the pancreas can leak digestive enzymes, causing severe pain, tissue damage, and systemic complications.
Types of Pancreatitis
- Acute Pancreatitis – Sudden inflammation, often caused by gallstones or alcohol abuse.
- Chronic Pancreatitis – Long-term damage leading to permanent scarring and loss of function.
Current Treatment Limitations
- Pain management (often opioids, which carry addiction risks)
- Enzyme replacement therapy (for digestion)
- Surgery (in severe cases)
- Dietary restrictions (low-fat, no alcohol)
These treatments manage symptoms but don’t always address the underlying inflammation and cellular damage. This is where red light therapy comes in.
What Is Red Light Therapy?
Red light therapy (RLT) uses low-wavelength red and near-infrared (NIR) light to penetrate the skin and stimulate cellular repair. It’s non-invasive, painless, and free of UV radiation.
How Does It Work?
RLT works through photobiomodulation—a process where light energy is absorbed by mitochondria (the cell’s powerhouses), boosting adenosine triphosphate (ATP) production. This leads to:
✔ Reduced inflammation
✔ Enhanced tissue repair
✔ Improved blood circulation
✔ Decreased oxidative stress
These mechanisms make RLT a potential game-changer for pancreatitis.
Red Light Therapy and Pancreatitis: The Science
1. Anti-Inflammatory Effects
Chronic pancreatitis involves persistent inflammation. Studies show RLT reduces pro-inflammatory cytokines (like TNF-α and IL-6) while increasing anti-inflammatory ones (like IL-10).
🔬 Study Highlight:
A 2018 study in Lasers in Medical Science found that NIR light reduced pancreatic inflammation in animal models, suggesting potential human applications.
2. Pain Relief Without Drugs
RLT has been shown to modulate nerve signals, reducing pain perception. This could help pancreatitis patients avoid opioid dependence.
🔬 Study Highlight:
A 2020 Journal of Pain Research review confirmed that RLT significantly reduces chronic pain in various conditions, including visceral pain (like pancreatic pain).
3. Enhanced Tissue Healing
Pancreatitis can cause fibrosis (scarring). RLT promotes collagen remodeling and cellular regeneration, potentially slowing disease progression.
🔬 Study Highlight:
Research in Photomedicine and Laser Surgery (2016) demonstrated that RLT accelerates wound healing and reduces fibrosis in damaged tissues.
4. Oxidative Stress Reduction
Oxidative stress worsens pancreatitis. RLT increases antioxidant enzymes (like superoxide dismutase), protecting pancreatic cells.
🔬 Study Highlight:
A 2019 study in Oxidative Medicine and Cellular Longevity showed that RLT reduces oxidative damage in pancreatic cells, improving function.
How to Use Red Light Therapy for Pancreatitis
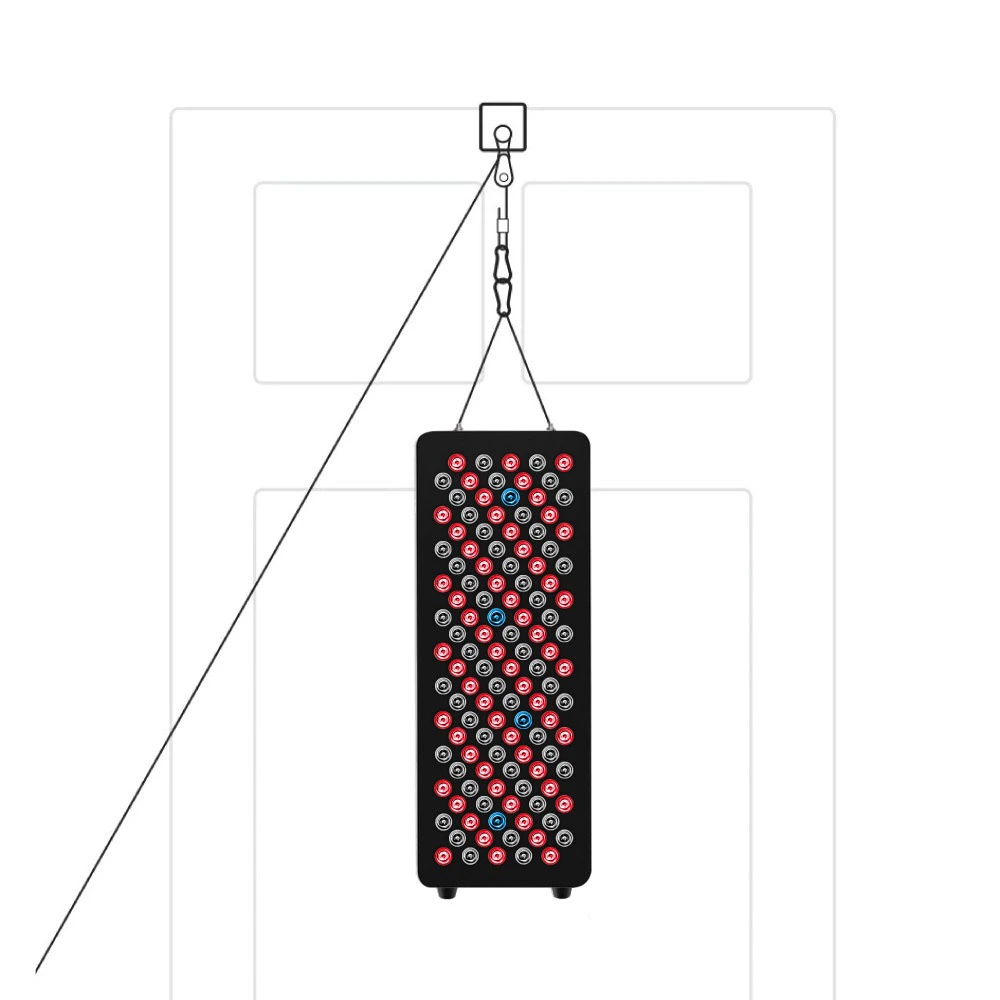
1. Professional vs. At-Home Devices
- Clinical-grade RLT (used in clinics) offers higher power.
- At-home devices (LED panels, belts) are convenient for daily use.
VELLGUS Elite V2
THE #1 RATED RED LIGHT DEVICE
VELLGUS pro V2
THE #1 RATED FULL BODY RED LIGHT DEVICE
2. Optimal Wavelengths
- Red light (630-670 nm) – Good for superficial tissue.
- Near-infrared (810-850 nm) – Penetrates deeper, ideal for pancreas.
3. Treatment Protocol
- Frequency: 3-5 sessions per week
- Duration: 10-20 minutes per session
- Placement: Over the upper abdomen (pancreas location)
Note: Always consult a doctor before starting RLT, especially if you have underlying conditions.
Safety and Side Effects
RLT is generally safe with minimal side effects. Rare cases report:
- Mild skin irritation
- Temporary eye strain (avoid direct eye exposure)
Unlike medications, RLT is non-toxic and non-addictive.
Future Research and Potential
While current studies are promising, more human clinical trials are needed. Researchers are exploring:
- Combining RLT with traditional treatments
- Optimal dosing for pancreatitis
- Long-term effects on pancreatic function
Conclusion: Is Red Light Therapy Worth Trying?
Red light therapy offers a safe, non-invasive, and scientifically backed option for managing pancreatitis symptoms. While it shouldn’t replace conventional treatments yet, it may serve as a powerful adjunct therapy to:
✅ Reduce inflammation
✅ Alleviate pain
✅ Promote healing
✅ Improve quality of life
If you or a loved one suffers from pancreatitis, discussing RLT with a healthcare provider could open new doors for relief.
Final Thoughts
The future of pancreatitis treatment may lie in innovative therapies like RLT. As research grows, we may see this light-based approach become a standard part of pancreatic care.
Would you try red light therapy for pancreatitis? Share your thoughts in the comments!
References
- Lasers in Medical Science (2018) – NIR light and pancreatic inflammation
- Journal of Pain Research (2020) – RLT for chronic pain
- Photomedicine and Laser Surgery (2016) – RLT and tissue healing
- Oxidative Medicine and Cellular Longevity (2019) – RLT and oxidative stress